Abstract
INTRODUCTION: Diffuse large B-cell lymphoma (DLBCL) is the commonest NHL subtype in sub-Saharan Africa (SSA), as in other parts of the world. Limited prospective data from the region have shown that DLBCL is curable in a substantial proportion of cases with chemotherapy and appropriate supportive care. However, little is known about costs of DLBCL treatment in the region.
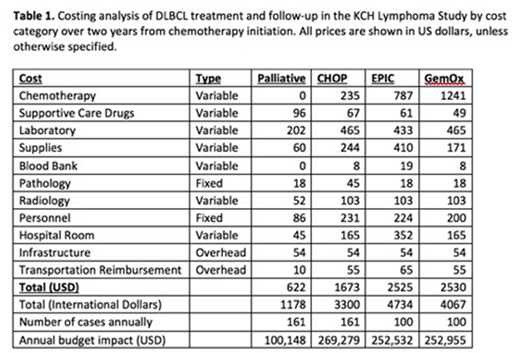
METHODS: We conducted a microcosting and budget impact analysis from a health systems prospective in Malawi, a low-income country in SSA. All costs were determined based on real-world costs for treating DBLCL patients at Kamuzu Central Hospital (KCH), a national teaching hospital in Lilongwe, Malawi, as part of a prospective, ongoing, longitudinal cohort study, the KCH Lymphoma Study. We calculated costs of care for palliative care only, first-line chemotherapy with cyclophosphamide, vincristine, doxorubicin, and prednisone (CHOP), and second-line chemotherapy for relapsed/refractory DLBCL with either ifosfamide, cisplatin, prednisone, and etoposide (EPIC) or gemcitabine and oxaliplatin (GemOx). Cost data were taken directly from costs paid for goods and services at KCH. Costs were calculated on a per-patient, activity basis, and total costs were estimated based on the average patient experience in our cohort through two years of care. Likewise, data from the KCH Lymphoma Study was used to estimate supportive care events and costs, including the number of hospitalizations during treatment for each type of chemotherapy delivered. Personnel costs were calculated based on interviews of clinic personnel, as well as actively observing time spent on clinical activities. Overhead costs consisted primarily of pathology and laboratory infrastructure and were amortized over 25 years. All costs were collected in, or converted to, 2017 USD using Malawian GDP deflator. Total cost is also shown in International Dollars to facilitate comparisons across countries. Finally, using national cancer registry data and data from the KCH Lymphoma Study, we calculated the annual budget impact for Malawi to treat all DLBCL cases.
RESULTS: All costs are shown on a per-patient basis (Table 1) using median chemotherapy cycles as received by the historical cohort of patients in the KCH Lymphoma Study, with follow-up visits for two years from chemotherapy initiation. Median number of chemotherapy cycles were as follows: CHOP (5), EPIC (3.5), and GemOx (5).
CONCLUSIONS: To our knowledge, this is one of the first studies to rigorously examine cost and budget implications of DLBCL care in SSA. We calculated that first-line chemotherapy with CHOP can be delivered for $1050 more per patient compared with palliative care alone in this single-institution microcosting analysis. Strengths include microcosting based on real-life costs derived from utilization data in this highly resource-limited setting. Although this single-institution study may limit generalizability, these data can help guide resource allocation for a common curable cancer throughout SSA. Planned analyses include an ongoing formal cost-effectiveness analysis to compare DLBCL treatment to other accepted health care interventions in SSA.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal